Antigen-Antibody Reaction: Definition, Properties, Stages, and Types
What is Antigen-Antibody reaction?
“During an immune response, the antigens and antibodies interact with each other, called antigen-antibody reaction.” It is also known as Ag-Ab reaction. This reaction occurs under highly specific conditions. An antigen reacts only with antibodies made by itself or similar antigens.
This reaction is essential for humoral or antibody-mediated immunity. It helps the body detect infectious agents and certain non-specific antigens, such as enzymes.
Properties of Antigen-Antibody reaction
- It is a visible reaction, meaning it can be observed directly.
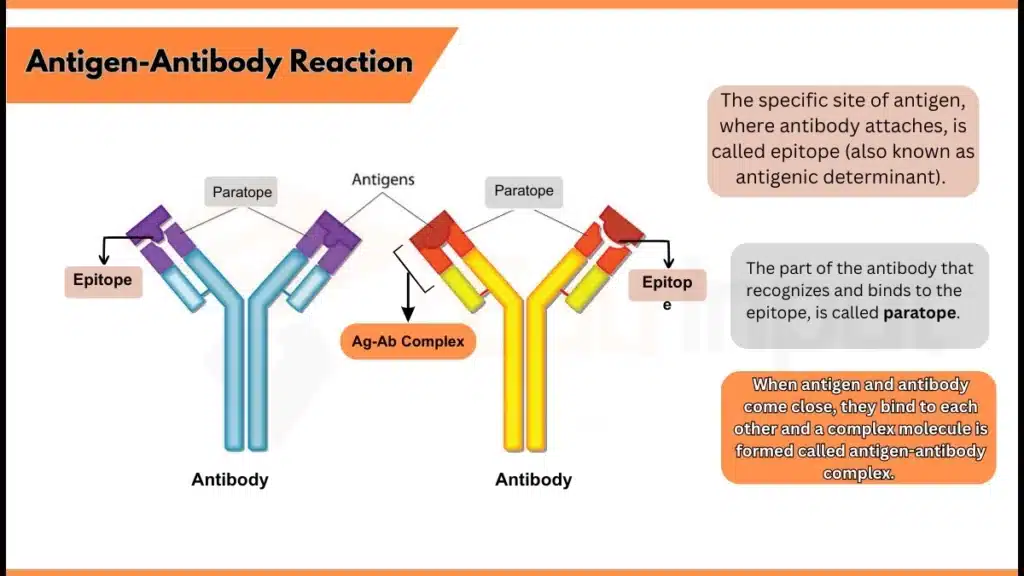
- When antigen and antibody come close, they bind to each other to form an immune complex, called Ag-Ab complex.
- The specific binding site of antigen, where the antibody attaches, is called epitope. While the binding part of the antibody is called paratope.
- The antigen-antibody reaction is highly specific, meaning an antibody binds only with the antigen, which causes its production.
- The antigen-antibody binding includes intermolecular forces, i.e. ionic bonds, hydrogen bonds, hydrophobic interactions, and Van der Waals forces.
- The antibody and antigen are not denatured. They maintain their original shape and function during and after the reaction.
- It is a reversible reaction.
- Affinity: It shows the strength of the bond between the antigen’s epitope and the antibody’s paratope, and is measured by affinity constant K.
- Avidity: It shows the total binding strength of the Ag-Ab complex. It involves affinity and the number of binding sites (valencies) on both antigen and antibody.
- Avidity measures how well an antibody binds to a multivalent antigen.
- A multivalent antigen has many epitopes (parts that trigger immune responses).
- Each epitope stimulates the production of a specific antibody.
- Different antibodies bind to the same antigen’s various parts (epitopes/determinants).
- Cross-Reactivity: Sometimes, an antibody binds to similar sites on different antigens. The antibody that performs this reaction is known as cross-reactive Ab.
- The bonds involved in cross-reactions are weak.
Stages of Antigen-Antibody reaction
The antigen and antibody reaction mostly happens in vitro (outside the body), called serological reaction. This reaction involves three different stages:
- The first stage includes binding antigens and antibodies to form an Ag-Ab complex.
- The second stage displays the visible results, such as precipitation or agglutination.
- The third stage involves the destruction or neutralization of antigens to prevent harm
Types of Antigen-Antibody Reaction
There are five types of antibody-antigen reactions, which are described below:
- Precipitation Reaction
- Agglutination Reaction
- Complement Fixation
- Immunofluorescence
- ELISA – Enzyme-Linked ImmunoSorbent Assay
1. Precipitation Reaction
When antibodies react with a soluble antigen in an electrolyte (salt like NaCl) at a specific pH and temperature, they form an insoluble complex called a ‘precipitate’. The antibody that causes this precipitate is known as precipitin, and the process is called the precipitation reaction.
Precipitation takes place in two media:
a) Liquid Precipitation
An antigen-antibody reaction is performed by adding a constant amount of antibody to many tubes, and then an increased amount of antigen is added to the tubes. The antibodies and antigens attach to each other and form a precipitate.
b) Gel Precipitation
In this method, plates or petri dishes are used with gels. Both the antibody and antigen spread (diffusion) freely through the gel in all directions. Based on the diffusion rate and number of reactants, they form a visible precipitate at a specific point.
2. Agglutination Reaction
The reaction in which an antibody binds with a particular (insoluble) antigen results in clumping, is known as agglutination. It occurs in the presence of electrolytes, suitable pH, and temperature. The antibodies that cause this reaction are called agglutinins, and the antigens that form these clumps are Agglutinogens.
Agglutination reactions involve the following types:
a) Slide Agglutination
This method is used to check the quantity of agglutinating antibodies. A uniform antigen sample is added to a drop of saline and antiserum on a ‘slide’. Then, the slide is mixed gently. If it shows the clumps, the test result is positive.
b) Tube Agglutination
In this method, the serum is diluted with saline in ‘test tubes’, adding a specific amount of antigen. A control tube without serum is also placed. The tubes are incubated, and the visible clumps appear. This test is used to diagnose several diseases.
c) Passive agglutination
This test is like the hemagglutination test, but the physical nature of the reaction is changed. Antigens are attached to particles like RBCs, latex beads, or bentonite. When these particles are added to the patient’s serum, agglutination occurs.
3. Complement Fixation
In this test, a complement system includes a group of 11 proteins in serum to check for the antigen-antibody reaction. In the first step, the serum is heated to 56°C (to inactivate its natural complement). Then, the test antigen (Ag) and serum are mixed with a known amount of complement and are incubated for 18 hours at 4°C. If the antibody (Ab) specific to the antigen (Ag) is present in the serum, an antigen-antibody complex is formed, which binds the complement,
4. Immunofluorescence
Fluorescence is the ability to absorb light with one particular wavelength and emit light with a different wavelength. Fluorescent dyes glow brightly when exposed to UV radiation as they convert UV light into visible light.
In 1942, Coons et al. described that fluorescent dyes, along with antibodies, can be used to detect antigens. For example:
- Fluorescein is a commonly used dye, which absorbs blue light of 490 nm and emits a bright yellow-green light of 517 nm.
- Phycoerythrin absorbs light effectively and is 30 times more efficient than fluorescein. It emits a bright red fluorescence. That’s why it is used widely as a popular label for immunofluorescence techniques.
5. ELISA – Enzyme-Linked Immunosorbent Assay
In 1971, some sensitive tools, like enzyme-labelled antigens and antibodies, were developed to detect antigens and antibodies. These tests are more safe and affordable than radioimmunoassay (RIA). In this process, a ligand molecule attached to the antibody is combined with an enzyme like peroxidase or alkaline phosphatase.
ELISA involves three types:
a) Indirect ELISA
This test is used to detect HIV. The proteins that are developed by recombinant technology are coated on a plate. Then, the patient’s serum is mixed with it to check the presence of antibodies.
b) Sandwich ELISA
This method detects antigens by using an antibody-coated plate. The sample is added, and a labeled antibody identifies the antigen. A color change indicates antigen levels, with greater intensity showing more antigen. Unbound antigen is washed away after the reaction.
c) Competitive ELISA
To measure antigen levels, the sample is mixed with an antibody and added to an antigen-coated plate. High antigen levels result in fewer antibodies binding to the plate, as they are already bound to the sample antigen. A secondary antibody linked to an enzyme is then used to measure the antibodies attached to the plate.
Applications of Antigen-Antibody reaction
Here are some main applications of antigen and antibody reactions:
- It helps identify blood groups for safe blood transfusions.
- Diagnosis of infectious diseases.
- Detecting certain proteins in blood
- Measurement of substances in the body through immunoassays.
- Detection of specific immune system disorders.



Leave a Reply